Steph Coelho is a freelance health writer, web producer, and editor based in Montreal. She specializes in covering general wellness and chronic illness.
Learn about our editorial processPublished on March 17, 2022Medically reviewedVerywell Health articles are reviewed by board-certified physicians and healthcare professionals. Medical Reviewers confirm the content is thorough and accurate, reflecting the latest evidence-based research. Content is reviewed before publication and upon substantial updates. Learn more.byJenny Sweigard, MD Medically reviewed byJenny Sweigard, MDJenny Sweigard, MD, is board-certified in internal medicine. She is an in-patient physician at Novant Health Huntersville Medical Center in North Carolina.
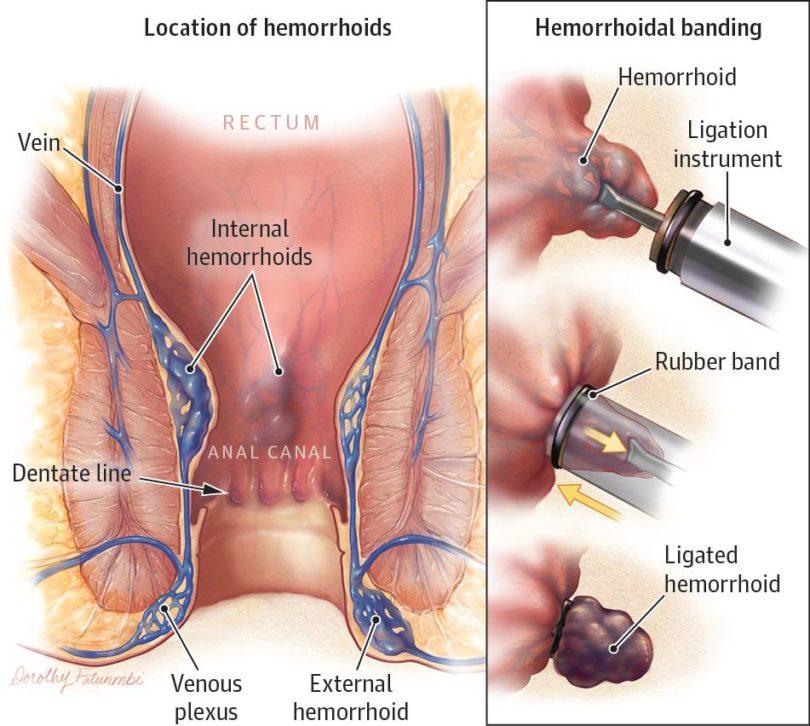
Learn about our Medical Review BoardTable of ContentsView AllTable of ContentsHemorrhoids are swollen veins that develop around the anus or inside the lower rectum. If you have recurring hemorrhoids that cause discomfort, you may want to consider medical treatment.
Surgeons use a surgical procedure called hemorrhoid banding to treat internal hemorrhoids (those located in the rectum). The treatment is also known as rubber band ligation. The medical procedure also helps prevent them from coming back.
This article takes a closer look at the hemorrhoid banding procedure along with alternative treatments for hemorrhoids.
Hemorrhoid banding is a medical procedure used to treat internal hemorrhoids. According to a 2019 study, banding is an effective and inexpensive way to treat hemorrhoid symptoms.
Your doctor may recommend a banding procedure if you have internal hemorrhoids that:
You’re at higher risk for developing hemorrhoids if you:
Before the procedure, a healthcare provider will likely ask you the following questions:
A Fleet's enema may be given before the procedure.
Healthcare providers typically perform this procedure in an outpatient setting, often right at the medical office.
During a hemorrhoid banding procedure, a surgeon will place a rubber band around any hemorrhoids inside your rectum. This cuts off blood flow, which shrinks the hemorrhoid, eventually causing it to disappear completely.
To perform the rubber band procedure, your healthcare provider will insert a special rubber banding tool through a speculum to band the hemorrhoid at its base. They may use a suction device or forceps to hold the hemorrhoid in place and place the rubber band.
Your doctor will use a local anesthetic to minimize pain during the procedure and immediately afterward. They may also prescribe you a topical ointment to help with post-operative discomfort.
The procedure likely won’t last very long, but timing depends on how many hemorrhoids you have.
It usually takes about a week for the hemorrhoid tissue to die and fall off.
In the meantime, you can expect some amount of pain in the week after the procedure. This will vary from person to person since we all have different pain thresholds. You may also feel a sense of anal fullness. Bleeding can also occur.
You may find it helpful to take over-the-counter (OTC) Tylenol (acetaminophen) to minimize any pain or discomfort you have after the banding procedure. Nonsteroidal anti-inflammatory drugs such as Advil (ibuprofen), Aleve (naproxen), and aspirin should be avoided for four to five days before and after the procedure as they may increase the risk of bleeding.
Another option for minimizing discomfort is to sit in a shallow tub of warm water, also known as a sitz bath. Taking stool softeners, staying well hydrated, and eating plenty of fiber can also help make bowel movements less painful.
It may take up to two weeks to heal and recover in some cases. And depending on the size and severity of the hemorrhoids, you may require multiple banding treatments to get rid of them entirely.
Early potential complications of this procedure include:
In the long-term, risks can also involve:
Because complications may be more likely in people with certain conditions. Your healthcare provider may recommend alternative treatments if you:
In some cases, the procedure may not be possible if there’s not enough tissue to apply a rubber band.
If at-home treatment and lifestyle changes don’t help your condition, your doctor may recommend the following medical treatments for hemorrhoids.
This procedure is also known as infrared photocoagulation. It involves using an infrared light beam to burn off internal hemorrhoids.
Electrocoagulation may be less painful than rubber band ligation because your doctor will need to perform less tissue manipulation during the procedure. However, evidence suggests that electrocoagulation isn’t as effective and may have a higher failure rate than banding.
This procedure involves injecting the vessels with a chemical solution to shrink and eliminate internal hemorrhoids.
Surgery (hemorrhoidectomy) is the most invasive procedure for treating hemorrhoids but is intended to eliminate them permanently. Surgeons typically perform this type of removal for hemorrhoids that have prolapsed (protruded from the anus) or very large external hemorrhoids that other treatments haven’t helped.
Hemorrhoid banding is an effective and non-invasive way to treat internal hemorrhoids. It can be done as an outpatient procedure in your healthcare provider's office. Banding cuts off circulation to hemorrhoids. The banded portion eventually falls off within a week, leaving you hemorrhoid-free.
You may experience some pain and discomfort during and after the procedure. For most people, healing takes about a week or so.
While hemorrhoids are generally nothing to worry about, they can cause discomfort. Banding is an effective way to treat internal hemorrhoids that are causing you grief.
Knowing what to expect from the banding procedure can make it less nerve-wracking. If you have any additional questions about what to expect, don’t hesitate to talk to your healthcare provider.
Was this page helpful?Thanks for your feedback!Gas pain? Stool issues? Sign up for the best tips to take care of your stomach.
You're in!Thank you, {{form.email}}, for signing up.
There was an error. Please try again.